Child and Youth Mental Health
The implementation of interRAI Collaborative Action Plans to improve outcomes for children and youth exposed to domestic violence
Introduction
The purpose of this project was to partner with service providers to identify needs and the specific developmental, emotional, and behavioural difficulties of children who have been exposed to Domestic Violence and Abuse (DVA). The research team sought to accomplish this through the implementation and evaluation of comprehensive screening linked to evidence-based care planning to integrate trauma-informed knowledge into practice and children and youth 4-18 years of age to provide improved access to trauma-informed care.
Using the interRAI Child and Youth Mental Health assessment system and related applications (ChYMH; Stewart, Hirdes et al., 2015; see also www.interRAI.org), from a trauma-informed care perspective, we sought to build capacity and sustainability by training professionals (e.g., nurses, social workers, child-care workers) who work within the community (e.g., at mental health agencies, hospitals and schools) to interrupt the cycle of domestic violence or abuse at multiple levels. Factors targeted for identified intervention were tailored to the individualized needs of children/youth and families and included a variety of care planning protocols such as attachment, parenting, caregiver distress, and family functioning. By providing knowledge mobilization (e.g., information and resources) to community-based organizations, the research team sought to provide new evidence based on applied research to support sustained, effective community-level programming. In addition to education, training and early identification of children exposed to DVA, this intervention was designed to reduce the cycle of abuse with children in a high-risk, low socio-economic community with the ultimate intent of reducing the likelihood of DVA.
The interRAI ChYMH was implemented and evaluated with respect to its ability to fill existing gaps by offering a holistic system to identify child/youth and family needs, so that evidence-informed care planning interventions can be employed in a timely, effective manner. This integrated system comprehensively assesses medical, developmental, social, family and psychiatric problems while delivering best practice clinical guidelines and strategies for intervention to support knowledge transfer and mobilization. Through a multi-modal, multi-sectoral, community-driven approach to intervention, several areas of risk and protection specific to a trauma-informed approach were targeted to circumvent DVA to foster improved health outcomes. This approach enhances early detection, prevention, monitoring and intervention of developmental issues and mental health problems, improves consistency and continuity of care and reduce the variations/complexities in diagnosis and care often associated with the use of multiple or inappropriate services. This, in turn, can lead to improved life outcomes thereby diverting children and families from pathways often leading to intergenerational abuse. As such, strong use of a comprehensive evaluation facilitates the implementation of sustained, effective community-level programs.
Background
Exposure to domestic violence and child abuse (i.e., physical, emotional, or sexual abuse or exposure to domestic violence) has significant consequences for children's mental health. Childhood maltreatment has been negatively associated with functioning across multiple domains: cognitive (e.g., Masson et al., 2016; Masson et al., 2015), academic (e.g., Fry et al., 2017; McGuire & Jackson, 2018), and socioemotional and behavioral (e.g., Stewart et al., 2022). Research has also found that children with trauma are more likely to utilize healthcare services and mental supports than children without any experiences of trauma (e.g., Daigneault et al., 2017). Moreover, child polyvictimization (i.e., exposure to multiple types and incidents of trauma; Stewart et al., 2021) is positively associated with greater levels of symptom presentation (Stewart et al., 2021), mental health service urgency (Marshall et al., 2020), and involvement with more than one service agency (Briggs et al., 2013). While community agencies have an important role to play in promoting mental health for these children, the lack of an evidence-based, trauma-informed framework limits this potential positive impact. Similarly, mental health agencies that provide services (e.g., behavioural interventions) with little recognition to the trauma that has been experienced, do not have the impact that they could otherwise have. Although interventions that promote early childhood health among children and youth exposed to DVA generate significant economic returns to society (Schweinhart et al., 2005), prior to this project, there was no systematic, coordinated delivery of mental health screening, assessment and intervention for high-risk children and their families.
The goal of this project was to utilize interRAI Child and Youth Mental Health assessment system and related applications (ChYMH; Stewart, Hirdes et al., 2015; see also www.interRAI.org) from a trauma-informed care perspective to not only provide developmentally appropriate support for community-based organizations with trauma-informed resources, but also to enhance and expand integration across community services that specifically emphasize collaborative models. Further, we sought to improve service integration by providing professionals from various service sectors with a common language using the interRAI ChYMH and its related trauma-informed care approach to service delivery.
Key activities and outputs (project audience)
- Child and youth mental health practitioners engaged in the interRAI Trauma-Informed Care training (n = 247)
- Mental health agencies across Southwestern Ontario (n=16)
- Young people aged 4-18 years exposed to DVA (n = 11,903)
Project Outcomes
Healthcare providers at participating agencies
-100% reported changes in knowledge and/or skills (n=110)
- 89% of professionals/service providers who found the knowledge products or events valuable (n=28)
- 75% of professionals/service providers reporting changes in behaviour (n=28)
Prior to, and upon completion of the standardized interRAI TIC educational training on the 30 interRAI ChYMH clinical care plans, multidisciplinary healthcare providers (e.g., clinicians, social workers, therapists) at participating mental health agencies completed the Attitudes Towards Trauma Informed Care questionnaire (ARTIC-45; Baker et al., 2016) that measure respondent’s attitudes towards trauma-informed care. The training took approximately 8 hours to complete varying across participants depending on their learning style and approach.
When investigating a pre-post outcome for using paired sample t-tests, the results highlighted that healthcare providers shifted their beliefs to: (a) reflect that the traits of their child and youth clients are more malleable and external; (b) focus more heavily on safety, flexibility and healthy relationships upon working with clients who have experienced DVA; and (c) a more empathetic approach to behaviours for clients who have been exposed to traumatic event. Lastly, results highlighted a significant change in health providers self-efficacy in terms of being able to meet the needs of a traumatized client. Overall the interRAI TIC training supported clinicians in mental health agencies in Ontario to change their belief and practice to a more favourable use of TIC with their child and youth, and guardian clients.
In addition, a subset of providers participated in focus groups/interviews. Providers shared that the training supported their use of TIC, helped with TIC implementation in their agencies, and encouraged advocacy for providing timely services to clients. The implications of these results emphasize that the interRAI TIC training has helped to change the landscape of care for children, youth and their guardians who have experienced domestic violence and abuse.
Organizational Changes
-100% of managers interviewed at participating agencies (n = 8) noted changes to organizational policy and practice.
Eight individual interviews were completed with project participants who held a managerial role and who oversaw the project at their respective agency. Three key findings at an organizational level resulted from healthcare providers participating in the project:
(a) Improved organizational policy and practice of trauma-informed care for children and youth impacted by trauma;
(b) Project participation facilitated appropriate early identification and referral for the child (and assisted with triaging and prioritization of the child/youth’s mental health needs); and
(c) Increased interest in widespread use of the ChYMH and TIC training to reduce redundancies in information collected from non-standardized assessments.
Child and Youth with a history of trauma at the time the interRAI ChYMH assessment was complete & who completed multiple interRAI ChYMH assessments (between 30 and 365 days later) after health professionals completing the trauma-informed care training.
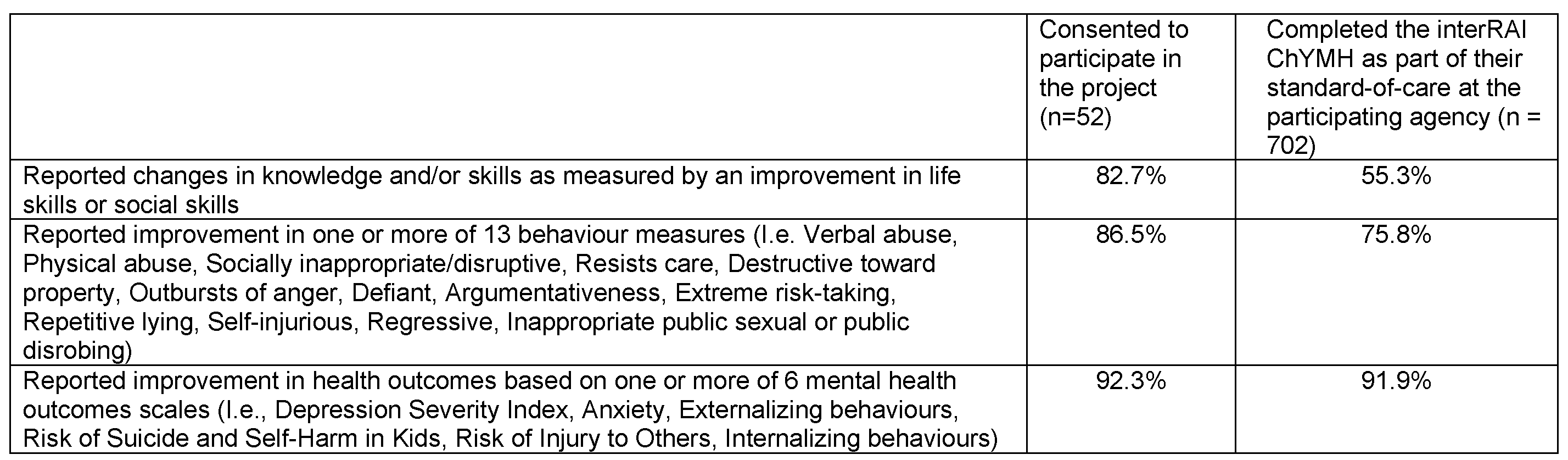
Findings from this project indicate that existing diagnoses, individual and relational strengths, age, sex, and service-provision factors are all important to consider with respect to impact on rates of improvement. Taken together, this highlights the need for a standardized, comprehensive assessment to properly evaluate needs and engage in care planning. Care planning includes gaining a comprehensive understand of the client’s trauma history/triggers/reactions, developing safety plans, identifying the level of threat the trauma reactions posed to the safety of the client, engaging in shared decision making and goal-setting, establishing safe and secure living arrangements, connecting clients with “safe adults”, practicing adaptive coping strategies, replacing maladaptive coping strategies with adaptive ones, conveying hope and empowerment and identifying and promoting resilient capacities.
Next Steps
Dr. Stewart and her team are actively seeking additional funding to foster a pan-Canadian uptake of the interRAI Child and Youth Mental Health Assessment, Trauma-Informed Care system. Several provinces across Canada (Prince Edward Island, Newfoundland and Labrador, British Columbia, Nova Scotia, and Manitoba) and internationally (e.g., India), have demonstrated interest in undertaking the interRAI ChYMH and TIC aspect respective to their provincial needs.
